Sleeping

Why am I tired all the time
Night terrors/nightmares
Many children have nightmares and night terrors, but most grow out of them. Some adults also can also have them.
Night terrors and nightmares are different and happen at different stages of sleep.
During a night terror you may talk and move about but are asleep. It's rare to remember having a night terror.
Nightmares are bad dreams you wake up from and can remember.
Night terrors are most common in children between the ages of 3 and 8, while nightmares can affect both children and adults.
| Night terrors | Nightmares |
|---|---|
| Mainly affect children | Affect both children and adults |
| Scream, shout, thrash about, jump out of bed, eyes open but not awake, will not remember it | Strong feelings of fear, child may wake up and be able to remember the dream |
| Happen in the early part of the night, sometimes more than once, lasting up to 15 minutes | Happen later in the night |
If you cannot move or speak as you wake up or fall asleep, you may have sleep paralysis. This is not the same as having a night terror.
Common causes of night terrors and nightmares include:
- being very tired or unwell
- sudden noises at night or needing to pee during the night (which can affect your deep sleep)
- something that's frightened you (such as watching a scary film) or made you stressed, anxious or worried
They can also be caused by:
- taking certain medicines, such as antidepressants
- conditions that affect sleep, such as restless legs syndrome or sleep apnoea
- mental health conditions, such as post-traumatic stress disorder (PTSD)
- conditions that affect the brain, such as dementia
Night terrors are more common in people with family members who have had night terrors or who sleepwalk.
See a GP if:
- your child has night terrors several times a night or has them most nights
- your child has lots of nightmares about the same thing
- you're having regular nightmares that are affecting your sleep and everyday life
For most people, night terrors and nightmares get better on their own.
If your child is having night terrors or nightmares, there are things you can try to help.
Do
try having a relaxing bedtime routine
keep a sleep diary (including things you did during the day and evening, how you were feeling and how you slept) to help identify any causes
try to deal with things that might be causing stress or anxiety
During a night terror, you should:
- stay calm and wait for the person to calm down
- do not talk to them or try to stop them moving about, unless there's a risk they could hurt themselves or someone else
- do not try to wake them – they may not recognise you and may get more upset if you try to comfort them
If they're having a night terror at the same time every night, try waking them up 15 minutes before the night terror every night for a week. This can sometimes stop the night terrors happening.
Treatment for nightmares in adults depends on what may be causing them.
If you're having nightmares caused by a traumatic event, a GP may recommend psychological treatment such as counselling.
If you have a condition that affects your sleep, treatment will usually involve trying to manage the condition better.
Sleep for primary aged children
We can offer you support if your child has difficulty sleeping. Lack of sleep in childhood can lead to irritability, forgetfulness, difficulties with learning and concentration, reduced ability to fight off infections, increased stress and difficulty regulating behaviour.
Our initial support consists of a virtual interactive presentation to support you with your child’s sleep to help them to develop healthy bedtime routines and sleep habits.
Once you have attended the initial session if the you or the practitioner identifies that the child may benefit from further support after the workshop, we will offer you two follow up sessions to plan and tailor interventions that will support you.
The sessions are usually weekly but would be planned to fit the needs of you and your child.
Each session would last about 45 minutes and be over a virtual platform- either in school or at home.
The sessions could cover subjects such as:
- Sleep cycle
- Tryptophan foods
- Melatonin production
- Bedtime routine
- A consistent approach seven days a week from the whole family
- Electronic gadgets/Screen time
- Bedroom environment
- Environmental/Sensory issues
- Talk time/worry box/worry journal/worry monster
- Inappropriate sleep associations
- Lighting
- Nightmares/Night terrors
- Sleep walking
Implementation of strategies for six months is required before a referral can be made to the sleep clinic for further assessment and medical support.
FAQs
What is melatonin?
Melatonin is the hormone that makes you sleepy. Melatonin is a natural chemical that is produced in our brain, it helps to regulate our body clock and the timing of when our sleep occurs. Melatonin level are affected by both light and temperature.
How long should a bedtime routine be?
Bedtime routine is the foundation for good sleep – it allows your child/young person to have an awareness of bedtime as it introduces the cues for sleep. The bedtime routine should last no longer than 45 minutes and should be consistent 7 days a week.
How many hours sleep should my child/young person have each night?

Is it true blue light/screens/gadgets can have an impact on sleep?
Modern LED screens omit short wavelength blue light. This light suppresses the natural production of melatonin and delays sleep onset. It’s recommended that screen time stops at least an hour before bed.
Why does my child take a long time to settle to sleep?
Your child may lack a consistent bedtime routine. Ensure your child is going to bed at an appropriate time.
Worries may impact on child’s ability to fall asleep. Work on one to one time during the day to lesson the anxiety around separation at bedtime.
Have a winding down time before bed, which may include breathing exercises or relaxation techniques.
Why does my child find it difficult settling to sleep, and why are they fussy re nightclothes?
Try heavier bedclothes (use blankets etc instead of duvet), or try laying a sheet or blanket over the duvet and tucking it well in to increase pressure of bedclothes on body or try a sleeping bag instead of covers.
Warm bedclothes in a tumble drier before putting child to sleep, so that the cold is not alerting them.
Cotton sheets often form little ‘tags’ with wear with can be very irritating to the child with high sensitivity to touch, try flannelette or towelling sheets instead. Acknowledge the child’s preferences for nightwear, some prefer tight fitting, others prefer very little.
Why does my child partially wake throughout the night?
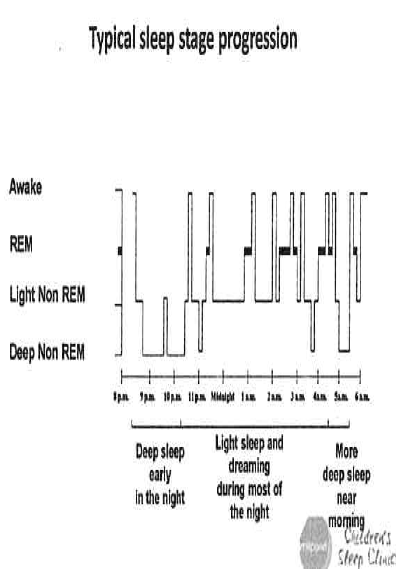
The diagram above shows the stages of sleep and how they differ throughout the night.
I have done all this before, what are you going to tell me that’s different?
The time may not have been right when you were implementing strategies before.
The strategies will take time, patience, commitment and consistency to implement effectively and see a positive behaviour change.
Working with our service will provide you with support and advice. By attending the tier one sleep webinar you may be reinforcing advice you have heard before.
You will gain a greater understanding of what can impact your child’s sleep.
Ensuring you have a good support network.
My child shares a room with siblings, how do I manage this?
Although this can present as a challenge you can implement a successful robust routine. It’s advised that Child A is settled to sleep first and 15/20 minutes later introduce Child B following the sleep strategy.
Do I have to be consistent at weekends etc. with routines?
Yes, it is very important to be consistent with both bedtime and wake up times.

School Health Service
Speak to the team for more information.
Need help now?
Text your school nurse on
07507 332473.
School Health virtual drop-in sessions
Apologies, our virtual drop-ins are paused at this time.
Need to speak to someone now?
Downloads
Give feedback
Have you used our services and want to give your views?
Kent Community Health NHS Foundation Trust
Local stakeholders
- Contact our Children's Integrated Therapy Service
- Contact our School Health Service
- Support services in East Sussex