Accessing our Children's Integrated Therapy Service
Accessing support
Our service is available for children and young people until they are 18 years old. Some of our pathways start at 3 years old, others start from birth and some go up to 19 if in fulltime education (see pre-referral guidance). We will support transition to adult services at an appropriate age and stage.
You can access universal, targeted and specialist support from Children’s Integrated Therapy and Equipment Service.
No referral is needed for universal and targeted support, which can be accessed by anyone working with the child or young person. These services include support via our website resources and training videos. Specialist support can be accessed by making a referral to the service.
We provide assessment and advice for school age children in East Sussex who are electively home educated or attend a private school with no onsite therapy service and fulfil our
Health needs and equipment needs for children in their home will be met through CITES regardless of school placement, for example, orthotics, postural management, toileting and
Where a child attends a private school that has its own onsite therapy service we work in partnership with the family and school therapy team where there are eating and drinking
To help you to get the right level of support, please follow our three step process:
1. Access our universal and targeted support offer
- Please choose from one of the seven pathways. On each page you will find short videos and longer training videos as well as resources and links to help children and young people progress with their learning and development. Please watch appropriate videos and implement recommended strategies.
- If your child/young person is of school age, we recommend that you discuss your concerns with your child’s SENCo. They will be able to advise you of what is already in place to support your child’s development.
- Watch our short video to get ideas on how to make your classroom inclusive for children with communication and sensory needs: CITES video tour - creating an inclusive environment in school (vimeo.com)
- Please choose from one of the seven pathways. On each page you will find short videos and longer training videos as well as resources and links to help children and young people progress with their learning and development. Please watch appropriate videos, use recommended resources and implement recommended strategies.
- Schools can find the East Sussex SEN Matrix at SEN Matrix | Czone and can access the Universally Available Provision document which sets out the provision that should be available to all children and young people so they can thrive in their setting by emailing sendqualityofeducation@eastsussex.gov.uk.
2. Refer to any specific pre referral guidance for each pathway
Children and young people can access this pathway from preschool age to 18 years old.
For speech sounds and selective mutism parents/ carers/school will need to supply evidence in the referral of strategies trialled from the resources available on the website over the course of 12 weeks, in order for the triaging therapist to determine if direct assessment is required.
You can also watch our ‘How to make a school years referral’ video for additional guidance, support and examples.
In addition
Speech sounds school years: Please use Speech Link® assessment and carry out the programme for two terms, you will be required to upload evidence of this, i.e. documents that show a baseline and evaluation of speech sound targets.
Voice: Children with voice problems are usually referred through ENT or other specialist tertiary centres. If there are concerns about a child’s voice quality (such as hoarseness, voice loss, etc.) this should be investigated via ENT services first.
Speech sounds early years: We consider referrals for speech sound difficulties from three years. Please send in our word list with your referral.
Cleft palate: Referrals usually come through tertiary services and are considered from birth where there are speech sound difficulties and/ or eating and drinking difficulties.
Stammering: Referrals are considered for stammering after 27 months. Many children experience non-fluency when they start to talk in phrases and sentences. Usually this non-fluency subsides within three to six months. If there is no sign that the fluency is improving after this time we recommend referral. Where the child is aware of the stammer we advise immediate referral.
Children and young people can access this Pathway from preschool age to 18 years old.
Parents/carers/school will need to supply evidence in the referral of strategies trialled from the resources available on the website over the course of 12 weeks, in order for the triaging therapist to determine if direct assessment is required.
You can also watch our ‘How to make a school years referral’ video for additional guidance, support and examples.
In addition
Hearing impairment
Children with hearing impairment are usually referred through Audiology or ENT or other specialist tertiary centres. If you think a referral may be needed, please contact the service on 0300 123 2650 for advice.
Language - Early years
We consider referrals from 27 months. Parents and carers of children under this age should access advice and support through our website and local Family Hub services. We consider referrals below the age of 27 months for children who have a diagnosed genetic syndrome and meet current referral criteria, for example, Di George syndrome, Down’s Syndrome.
The SEND Early Years Service (SEND EYS) and Children’s Integrated Therapy and Equipment Service, Speech and Language Therapy (CITES SLT) have worked together to develop a joint pathway for early years children who have not yet developed a functional communication system and meet our respective services referral requirements.
Children without a functional communication system who meet the referral criteria will start their communication journey with SEND EYS; during the nursery year the SEND EYS will support early years settings to use graduated therapy programmes co-produced with CITES SLT to develop joint attention, early interaction, and introduction of signs and symbols to support intentional communication. This will be alongside a number of co-delivered workshops; Therapy One Point will support the same co-produced programmes.
At the end of their nursery year the SEND EYS will share children’s details with CITES SLT of any children on their caseload who continue to meet their referral criteria so that they can be taken on to CITES caseload. CITES SLT will provide a pre-school package of care including transition support. This package of care will include one-to-one sessions, information meetings, workshops co-delivered with SEND EYS and telephonic support through Therapy One Point when required.
Language - School years
Please use Language Link® assessment and carry out the programme for two terms, you will be required to upload evidence of this, for example, documents that show a baseline and evaluation of language targets.
Children and young people can access this Pathway from 3 years old to 18 years old (or up to 19 if in full time education).
School age - Please complete Zones of Regulation sessions, you will be required to upload evidence of this. If you are thinking a referral may be needed please contact Therapy One Point 0300 123 2650 to discuss the child before taking this step.
Children and young people can access this Pathway from 3 years old to 18 years old (or up to 19 if in full time education). We are not commissioned to provide interventions for children with sensory processing difficulties under age of three unless they are under a specialist Tertiary Centre such as Evelina Children’s Hospital or Great Ormond Street Hospital for sensory processing difficulties.
Parent/carers/school will need to supply evidence of strategies trialled from the videos and resources (see our pathways page) over the course of at least 12 weeks, in order for triaging therapist to determine if direct assessment is required.
In addition:
Motor skills (including Developmental coordination disorder): Please complete Jump Ahead and/or Sensory Circuits programme, for a minimum of three times a week for four academic terms, you will be required to upload evidence of this. If you are thinking a referral may be needed please contact Therapy One Point 0300 123 2650 to discuss the child before taking this step. A referral will be considered where children have accessed the Jump Ahead and/or Sensory Circuit programme but there are still ongoing difficulties such as: sequencing movements, spatial awareness, body awareness, motor planning.
Sensory skills: Please complete Sensory circuits programme, you will be required to upload evidence of this. If you are thinking a referral may be needed please contact Therapy One Point 0300 123 2650 to discuss the child before taking this step.
There should be evidence of severe sensory processing difficulties in at least three defined areas of self-care or activities of daily living such as using cutlery, managing buttons, dressing, toileting difficulties, pencil grip or personal hygiene. Attention does not count as an activity for daily living.
Children and young people can access this Pathway from 0 to 18 years old (or up to 19 if in full time education).
Parent/carers/school will need to supply evidence of strategies trialled from the videos and resources (see our pathways page) over the course of at least 12 weeks, in order for triaging therapist to determine if direct assessment is required.
Please complete Jump Ahead and/or Sensory Circuits programme, for a minimum of three times a week for four academic terms, you will be required to upload evidence of this. If you are thinking a referral may be needed please contact Therapy One Point 0300 123 2650 to discuss the child before taking this step.
In addition:
Hypermobility: Please contact Therapy One Point if hypermobility has a significant impact on gross motor functional ability, for example, causing sleep disturbance on a regular basis or impacting on attendance at school.
Children and young people can access this pathway from 0 to 18 years old (or up to 19 if in full time education).
This pathway would be chosen over Moderate disability in cases where the following will be primary area of need:
- Complex health needs
- Multiple specialist interventions
- Cerebral Palsy - levels 4-5 of the Gross Motor Function Classification System
- eating and drinking difficulties (dysphagia)
- Profound and multiple learning disability
- Neuro-muscular (acute deterioration or new complex presentation)
- Susceptibility to respiratory compromise including that associated with eating and drinking difficulties (cognition, airway clearance, decreased active movement and limited cough).
In addition:
Musculoskeletal problems
Children with musculoskeletal problems should be referred to the appropriate Musculoskeletal (MSK) Physiotherapy Service. We do accept referrals for babies with musculoskeletal problems, this could include the following:
- congenital foot abnormalities e.g. Talipes (club foot)
- preferential head turning (Torticollis)
- hip dysplasia (DDH)
- shoulder dystocia with apparent neuromuscular signs (Erb’s Palsy).
Eating and drinking
Some children need specialist support from a speech and language therapist or occupational therapist to support their swallow safety and functional eating and drinking skills.
It is important to consider that children may present with behavioural feeding difficulties such as gagging on specific textures, inflexibility around mealtimes, aversive behaviours around temperature of foods, colour of foods, texture of food and smell of food. Referrals for children who only have behavioural difficulties in relation to eating and drinking would not usually be accepted. However, we can offer advice on some sensory eating and drinking strategies.
Consider a referral for children showing the following signs:
Birth to six months:
- baby has difficulty establishing or maintaining a rhythmical suck swallow and breath pattern with appropriate pacing, resulting in: coughing, choking, colour change or nasal regurgitation.
- baby is distressed when feeding or straight afterwards, they may also vomit a lot, draw legs up in pain, unable to suck on a teat, weight loss, speak to GP, then refer
- arching or stiffening of the body during feeding (affecting feeds)
- irritability or lack of alertness during feeding
- long feeding times (more than 30 minutes)
- Difficulty establishing breastfeeding.
- Difficulty establishing a latch onto nipple/teat.
From six months to adult may also include:
- difficulty chewing
- coughing or choking during meals
- food or liquid coming out of the mouth or nose
- difficulty coordinating breathing with eating and drinking
- gurgly, hoarse, or breathy voice quality
- frequent spitting up or vomiting (in combination with other signs)
- recurring pneumonia or respiratory infections
- less than normal weight gain or growth (in combination with other signs)
- eating and drinking difficulties as a result of degenerative condition.
Downs syndrome
All babies with Downs syndrome should be referred by their Health Visitor at approximately six months. The service will then arrange a therapies advice and monitoring session. Children are entitled to a further session in their pre-school year to ensure a smooth transition into school. If a child has a therapy need at any other time, for example, eating and drinking or equipment needs, they can be referred on the basis of their needs.
Special school
For teachers and parents/carers of pupils in special school, please initially discuss your concerns with the therapists that regularly visit the school. They will be able to discuss your concerns and arrange a review of the pupil’s needs if required.
Children and young people can access this Pathway from preschool age to 19 years old.
Please visit our adaptations page for further information.
3. Make a specialist referral if required once universal and targeted strategies are in place
0300 123 2650 if further advice is needed before making a specialist referral.
Having completed these three steps, you will then be ready to make a referral for a specialist pathway if required.
Referrals are triaged into seven specialist pathways to address specific needs. This is based on a child or young person’s profile of need rather than their setting or diagnosis. These seven pathways allow flexibility across all levels of service provision at any one time.
Further information
Age criteria
Children and young people from birth to 18 years but transition to adult services would occur within that time at an appropriate age and stage. Age 16 to 19 (up until young person 19 – last day of 18) if in full time education in East Sussex.
Full time education includes post-16 colleges that are equivalent to secondary school education.
For colleges that have therapy provision as part of their offer, the college therapist would meet the needs of the students.
In scope
- moderate to severe global development delay
- neurological conditions affecting development and posture such as cerebral palsy, muscular dystrophy
- rehabilitation following multi-level surgery who are known to CITES
- acquired brain injury, for example post encephalitis/near drowning, note this does not include intensive rehabilitation and children and young people should be ready for discharge to community therapy
- oncology
- palliative care
- syndromes affecting neurological development
- developmental co-ordination disorder (DCD) – subject to DCD pathway criteria
- eating and drinking difficulties relating to neurological developmental
- respiratory conditions that require teaching of clearing of secretions such as cystic fibrosis
- orthotic provision for children on active CITES caseload
- contribute to paediatrician led ASD diagnostic pathway for children in primary education
- language – subject to completion of specified programmes in settings and schools
- phonological disorder
- developmental verbal dyspraxia
- voice disorders
- hearing impairment
- cleft palate and non-cleft velo-pharyngeal insufficiency
- dysfluency
- selective mutism
- augmentative and alternative communication
- juvenile idiopathic arthritis
- Talipes/Ponseti
- hip dysplasia/Pavlik harness
- severe hypermobility if condition is significantly impacting on gross motor functional ability
- Torticollis
- Erb’s palsy
- post orthopaedic surgery for children on CITES caseload with pre-existing developmental or neurological condition
- chronic fatigue syndrome/chronic regional pain syndrome – where children are under the primary care of CAMHS/ primary mental health services
- severe sensory processing difficulties in children over three years, affecting function in at least three defined areas of self-care or activities of daily living. Please note this does not include attention in the classroom
- serial casting post Botox.
The emphasis of occupational therapy is enabling. This means helping children to overcome functional difficulties that affect daily life and may present at home or in the school environment.
Referrals are specified for children who present with significantly delayed motor development which impacts on their daily functioning. This includes children with an underlying neurological condition, motor-planning difficulties, global developmental delay, ASD (where skills are not in line with diagnosis), upper-limb dysfunction, palliative care and life-limiting conditions. There is an expectation that all school-age children access the Jump Ahead programme, designed to address fine/gross motor skill acquisition and sensory circuits (sensory-motor programme) at school before a referral is considered.
Postural management
Occupational therapists work with the child and family to identify appropriate seating systems or equipment to support 24-hour postural management of children with complex physical disabilities. Seating can range from low level postural support to complex, dynamic modular seating systems. Similarly, occupational therapists will work closely with their physiotherapy colleagues in relation to prescription of sleep systems to make sure correct positioning at night time.
Activities of daily living
Occupational therapists are able to identify and work with children to identify the underlying difficulties preventing a child from being as independent as possible in areas of self-care. Interventions may be in the form of a programme, advice, direct intervention from an occupational therapist or integrated therapy assistant under the guidance of the treating therapist or by adapting an activity to meet the needs of the child. Interventions may include the following:
- dressing, use of techniques such as backward chaining to support skill progression
- eating and drinking, for example use of cutlery, dycem (non-slip mat), plate-guards and activities
- access to suitable bathing/ toileting facilities.
Equipment/minor adaptations to support daily living
Occupational therapists may provide equipment to facilitate independence either in the home or to access education. Interventions may include the following:
- access to bathing/showering: Bath-lifts, bath-boards, grab rails and shower-chairs
- toileting: Commode, toilet-frames, specialist modular toileting systems
- manual-handling equipment such as mobile hoists, transfer-boards, slide sheets.
Adaptations (birth to 18)
Please note, over 18s should be referred to Adult Social Care.
For children with complex physical disabilities or challenging behaviours compromising their safety in the home, there may be a need to adapt the home and/or school environment. Major adaptations are subject to criteria set out in the Disabled Facilities Grant legislation and the budget is held by local councils. Occupational therapists are responsible for assessing need under this legislation and making clinical recommendations regarding reasonable adaptations to meet a child’s needs. It is not always possible to provide a solution within the grant funding, in such cases the occupational therapist will work with the wider multi-agency team to support a family with exploring re-housing options.
Motor co-ordination difficulties which severely affect functional daily living
A referral will be considered where children have accessed the Jump Ahead programme or Sensory Circuit programme but there are still ongoing difficulties such as:
- sequencing movements
- spatial awareness
- body awareness
- motor planning.
Evidence is required where a child has been unable to progress and Jump Ahead should be completed a minimum of three times a week for four academic terms.
Visual perception
Visual motor integration impacts on handwriting and letter formation. Please note we do not deliver handwriting programmes but will assess and advise schools regarding implementation of appropriate programmes where applicable.
Sensory processing
There should be evidence of severe sensory processing difficulties in at least three defined areas of self-care or activities of daily living such as using cutlery, managing buttons, dressing, toileting difficulties, pencil grip or personal hygiene. Attention does not count as an activity for daily living. We are not commissioned to provide interventions for children with sensory processing difficulties under age of three unless they are under a specialist Tertiary Centre such as Evelina Children’s Hospital or Great Ormond Street Hospital for sensory processing difficulties.
Upper-limb
Where applicable OT will provide upper-limb programmes to promote function and development of self-care. Complex cases such as children with neurological impairment may be provided with a thumb or wrist splint where appropriate.
Neurological concerns or conditions affecting development
Please refer for any of the following:
- all children with a new diagnosis of Cerebral Palsy (CP) or showing signs of an evolving motor disorder
- children moving into the area with an existing diagnosis of CP who have functional difficulties
- babies and children presenting with any of the following:
- abnormal tone
- asymmetrical movement or unusual movement patterns. W sitting, bottom shuffling and in-toeing are not indications of an abnormal movement pattern unless abnormal tone is present
- functional difficulty for example difficulty standing or walking and out of line with normal developmental parameters
- delayed milestones or poor quality of movement
Acquired brain injury
CITES do not deliver intensive rehabilitation. The child should be ready for discharge to community therapy services
Neuromuscular conditions which involve a progressive loss of functional motor skills such as Charcot Marie Tooth, Spinal Muscular Atrophy, metabolic disease, muscular dystrophy)
Treatment and frequency will vary depending on the age and the stage of the child.
- all children with a new diagnosis of neuromuscular disease
- early years children with a plateau of gross motor development for more than six months
- children demonstrating a regression or loss of motor skills
- post orthopaedic surgery related to their condition
Developmental concerns including moderate to severe global developmental delay and syndromes
Please see developmental table below. Developmental norms are taken from Mary Sheridan, Birth to Five Years. 4th Edition.
Please note: Bottom shuffling is not an abnormal movement pattern. Many children who bottom shuffle instead of crawling to move around the floor start walking at a later age.
| Activity | Usual milestone | Refer to Physiotherapy |
| Independent floor sitting | five to nine months | 10 – 12 months |
|
Independent rolling - From front to back From back to front |
five to six months six to seven months |
eight to 10 months (may need referral to physiotherapy earlier if there is a concern about head control) |
| Pulling to stand | seven to 12 months | 13 – 16 months |
| Cruising around furniture | nine to 16 months | 17 – 20 months |
| Independent walking | nine and a half to 17 and a half months (children who bottom shuffle are usually delayed in walking 17 – 28 months) | 18 ½ months |
| Jumping | two and a half to three years | four years (a child who is not jumping at three is likely to have been known to the service previously for delayed walking) |
| Climbing stairs | three years (up and down holding a hand or a rail, usually two feet per step) | four years (a child who is struggling with stair climbing at three is likely to have been known to the service previously for delayed walking) |
Developmental coordination disorder
Children with motor coordination difficulties would be seen either by an occupational therapist or physiotherapist. Please see OT guidance on motor coordination difficulties for more information.
Toe walkers
The service would not normally accept referrals for toe walkers with no obvious neurological signs. Children should be referred if:
- there is asymmetry
- not possible to achieve 90 degrees at the ankle and there are associated developmental concerns or altered muscle tone. Where there are no associated concerns, or if the toe walking is intermittent then referral to musculoskeletal physiotherapy service provided by East Sussex Healthcare Trust is more appropriate
- toe walking with unusual body posturing or movement.
In-toeing
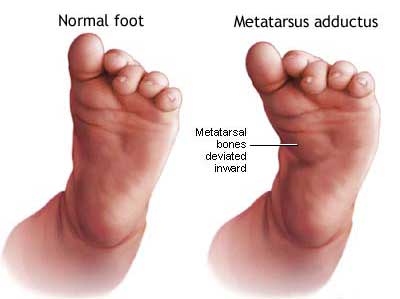 It is very common for young children’s feet to turn in when they walk. This is a common normal variant.
It is very common for young children’s feet to turn in when they walk. This is a common normal variant.
Referral to physiotherapy is only indicated if there is:
- significant asymmetry
- pain
- metatarsus adductus where it is not possible to passively correct the position of the forefoot to midline.
Orthotics
This provision is only for children already on the CITES caseload. No physiotherapy intervention is indicated in children with flat feet or feet that turn out. If pain is present then a referral to podiatry services provided by East Sussex Healthcare Trust is advised.
Musculoskeletal problems
Children presenting with musculoskeletal problems should be referred to the appropriate Musculoskeletal (MSK) Physiotherapy Service.
We do accept referrals for babies with musculoskeletal problems this could include the following:
- congenital foot abnormalities e.g. Talipes (club foot)
- preferential head turning (Torticollis)
- hip dysplasia (DDH)
- shoulder dystocia with apparent neuromuscular signs (Erb’s Palsy)
Chronic fatigue syndrome and chronic regional pain syndrome
Children with chronic fatigue syndrome and chronic regional pain syndrome can only be referred to CITES physiotherapy where they are under the primary care of CAMHS. Physiotherapy can advise on graded exercise and pacing of activities.
Hypermobility
Only refer to CITES physiotherapy when the condition is significantly impacting on gross motor functional ability such as causing sleep disturbance on a regular basis or impacting on attendance at school.
Juvenile idiopathic arthritis
Referrals are accepted for children with functional difficulties at home or at school who require advice on long term management of their condition.
Respiratory conditions
Please discuss all referrals requiring physiotherapy intervention for respiratory difficulties on an individual basis. Currently CITES is not commissioned to carry out this work.
If you are still unsure whether or not your referral will be accepted, please ring our Therapy One Point on 0300 123 2650.
Make a referral
Complete our form to make a referral into our Children's Integrated Therapy Service.
This form will open on the www.kentcht.nhs.uk website.
About
Give feedback
Have you used our services and want to give your views?
- Tell us your experience of using our NHS services
- Feedback about our website? Email us kentchft.eastsussexchildrenwebsitefeedback@nhs.net
Kent Community Health NHS Foundation Trust
Local stakeholders
- Contact our Children's Integrated Therapy Service
- Contact our School Health Service
- Support services in East Sussex